Prostate Disease
PROSTATE GLAND
The prostate is a walnut-sized gland located at the opening of the bladder in men. The main function of the prostate is production of seminal fluid, which is important for support of the sperm to aid fertility. The prostate has receptors which increase the size of the gland when stimulated by testosterone. The prostate is prone to various conditions including infection and inflammation (prostatitis), cancer and enlargement.
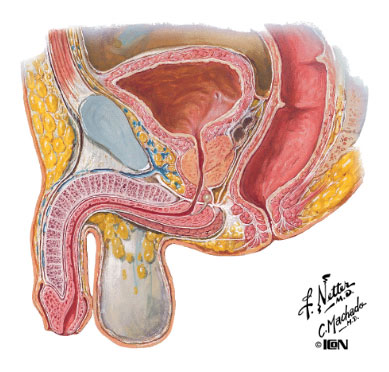
Male Pelvis
PROSTATE CANCER
Prostate cancer is the second most common cancer of men, and a leading cause of cancer-related death. The prevalence of prostate cancer increases with age.
The exact cause of prostate cancer is unknown, but genetic (inherited) factors appear to play a role in some men. Men who eat a high-fat diet, as well as black Americans, also have a higher risk of developing prostate cancer.
Prostate cancer has little or no symptoms in its early stages, and is often identified by a screening blood test (PSA - prostate specific antigen) and digital rectal examination (DRE). After discussion with your local doctor or Dr Bariol, you may wish to undergo PSA testing. Prostate screening is particularly important in men who have a family member or relative who has had prostate cancer, as their risk of also developing prostate cancer is up to 4 times greater.
The PSA is a useful test but only a biopsy can confirm the presence of prostate cancer. This is performed using a transrectal ultrasound (TRUS) to guide the biopsy needle into appropriate sections of the prostate. Usually 10-14 specimens of prostate tissue are removed and analysed by a pathologist to determine the presence of cancer. Prostate cancer may also be diagnosed incidentally when prostate tissue is removed during surgery to reduce the size of the gland (TURP - see below).
Managment of prostate cancer
Prostate cancer is staged according to its volume and extent of invasion or distant spread, and graded according to how biologically aggressive the cancer appears. Using this information, Dr Bariol will advise on a course of treatment. Usually you will have some choice as to how you are treated, and Dr Bariol will give you information to read and discuss all your treatment options so that you may make an informed decision.
Treatments for prostate cancer include active surveillance, surgery (radical prostatectomy) and radiotherapy (external beam or brachytherapy), and hormone therapy.
Active surveillance is reserved for men with low grade and volume cancer, or older men with other more serious medical illnesses. The cancer is monitored by means of DRE and PSA testing every 3-6 months, with TRUS biopsies every 1-2 years depending on the stability of the condition. If the volume and grade remain stable, it may be possible to avoid more active intervention altogether. However a change in the grade or volume of disease will usually lead to more aggressive treatment. A number of studies have shown this to be a safe approach.
Radical prostatectomy is surgical removal of the prostate through an abdominal incision (open retropubic radical prostatectomy) or keyhole surgery (laparoscopic or robotic radical prostatectomy). The prostate is removed along with the adjacent seminal vesicles and pelvic lymph nodes (if necessary). This operation reqauires a 3-4 day stay in hospital. Because the prostate lies between the bladder and the urethra, this area must be repaired to maintain continuity of the urinary stream. A silicone catheter is left in the penis for 7-10 days until this junction has healed. Radical prostatectomy carries a risk of urinary incontinence and erectile dysfunction, due to the proximity of the urinary sphincter and erectile nerves that control these functions.
Robotic assisted radical prostatectomy is an exciting new surgical technique which offers enhanced vision and precision, and has largely replaced pure laparoscopic prostatectomy. Its advantages over open radical prostatectomy are through less bleeding and more rapid convalescence. Functional bnefits with better continence and erectile function, have also been reported by some researchers. Dr Bariol is currently undergoing robotic training and hopes to offer this service to his patients by the end of 2013.
Radiotherapy is another effective form of treatment for prostate cancer, supervised by a radiation oncologist. Radiation can be delivered through the skin (external beam radiotherapy) or via temporary (high dose rate) or permanent (low dose rate, seeds) brachytherapy implants. Radiotherapy implants enable a higher dose, which increases the likelihood of cure, with fewer side effects as the radiation acts primarily on the prostate and less so on the surrounding organs. Suitability for this from of treatment depends on the stage and grade of cancer, prostate volume and the presence of bladder outflow obstruction.
Hormone treatment
Occasionally cancer cells can leave the prostate and spread (metastasise) to other parts of the body, especially lymph nodes and bones. In this situation, local treatment is often abandoned in favour of systemic drug treatment. Because prostate cancer cells rely on testosterone, drug treatments block the production of testosterone. This will usually give excellent disease control for several years, providing relief of symptoms and lowering the PSA considerably. Side effects include hot flushes, weight gain, tiredness, reduced libido and osteoporosis. Sometimes alternative forms of treatment are required as the cancer progresses in spite of hormone deprivation, including chemotherapy and drugs to enhance bone health.
BENIGN PROSTATE ENLARGEMENT
Benign prostate enlargement (BPE) refers to a non-cancerous growth of the prostate. This is brought about by the effects of ageing along with testosterone, the male hormone, which stimulates receptors on the prostate to make it grow.
BPE is the most common cause of difficulties with urination (lower urinary tract symptoms, LUTS) as men grow older. As the prostate enlarges, it interrupts the flow of urine, causing a reduced stream, hesitancy and terminal dribbling. Men with BPE may have to strain to empty their bladder, or have the feeling that the bladder does not empty completely when they pass urine. The muscle in the bladder (detrusor) tries to compensate for the increased resistance to voiding, which occurs as the prostate enlarges. The detrusor muscle becomes thicker (trabeculated), to try to maintain bladder emptying, however this may be at the expense of secondary irritative symptoms such as frequency and night-time urination (nocturia).
Not all men with BPE require treatment. Indeed as men get older, their prostate inevitably enlarges, but not all men complain of difficulties with urination. Why is this the case? This was poorly understood for some time, but we now realise that there is a dynamic, muscular component to BPE which is independent of the prostate's volume, so that symptom severity is not proportional to the size of the gland. Although some of the obstruction is due to increased size of the prostate, the increased muscle in the prostate is another important factor. When this muscle contracts, sometimes a result of cold or anxiety, the obstruction may become worse, making it even more difficult to pass urine.
Management of BPE
Unfortunately lower urinary tract symptoms are often non-specific and may reflect a variety of potential diseases. Accurate diagnosis of the underlying problem requires further investigation with blood and urine tests including PSA, micro-urine and urine cytology; flow study and ultrasound, which measures the speed with which you pass water, and the volume of urine left behind in the bladder afterwards (residual); and occasionally a cystoscopy, which is an examination of the urethra and bladder using a narrow instrument passed through the eye of the penis.
Cystoscopy
Treatment of BPE is reserved for men with bothersome urinary symptoms or those who develop complications of BPE including urinary tract infections (UTIs), blood in the urine (haematuria), bladder stones, complete inability to pass urine (urinary retention), overflow incontinence or kidney damage due to poor bladder emptying and back pressure on the kidneys (hydronephrosis). Both medical and surgical treatments are available.
Medical treatment for BPE
Alpha-blockers are the mainstay of medical (drug) treatment. These are medications which relax smooth muscle, including that muscle which surrounds the prostate and bladder neck. There are various alpha-blockers available with different degrees of specificity for the prostate smooth muscle. The less selective alpha-blockers also relax smooth muscle around veins, which can lower blood pressure and cause dizziness at higher doses. Selective alpha blockers have fewer side effects but are more expensive.
Other medications for BPE include finasteride, which works slowly to reduce the size of the prostate, and herbal remedies including serenoa repens.
Surgical treatments for BPE
The principles of surgery for BPE are to produce a cavity or channel within the prostate to allow urination without obstruction. There are two main techniques available.
Transurethral resection of prostate (TURP, or "rebore" procedure): this uses heat through an instrument (resectoscope) inserted through the penis to carve small "chips" of tissue from the middle of the enlarged prostate. The prostate is remodelled to allow unobstructed voiding. A catheter is left for 1-2 days until the urine clears. Hospital stay is only 2-3 days but you will need to restrict yourself to light activities for a few weeks after surgery. Flow rate usually improves rapidly after surgery, but the need to pass urine frequently may take a few months to subside.
TURP Middle Lobe
Laser prostatectomy: this technique uses laser energy to remove or vaporise the inner, overgrown part of the prostate gland. There tends to be less bleeding than in TURP, which allows patients a faster recovery and shorter period of catheterisation. This technique is suitable for men using blood-thinning agents (such as aspirin or warfarin) for heart attack or stroke prevention.
Precision Beam
Dr Bariol will be happy to discuss your treatment in detail at the time of your consultation.